Acute Pancreatitis
- Acute Pancreatitis
- Recurrent Acute Pancreatitis
- Chronic Pancreatitis
- Autoimmune Pancreatitis
- Familial Chylomicronemia Syndrome
- Pediatric Pancreatitis
What is Acute Pancreatitis?
Acute Pancreatitis (AP) is a sudden inflammation of the pancreas, a gland behind the stomach that plays a key role in digestion and blood sugar regulation. Normally, the pancreas produces digestive enzymes that are activated in the intestine to help break down food, along with hormones like insulin to manage blood sugar levels.
In acute pancreatitis, however, these enzymes become activated before they can leave the pancreas, causing the gland to “digest” its own tissue. This self-digestion triggers inflammation, intense pain, and in severe cases, life-threatening complications. The severity of acute pancreatitis can vary, ranging from mild discomfort to a critical condition that requires urgent medical attention.
Prevalence
Acute pancreatitis is the leading cause of gastrointestinal-related hospitalization in the United States, with over 200,000 hospital admissions each year. It is becoming more common, not only in the U.S., but worldwide. Over the past two decades, the number of acute pancreatitis cases per 100,000 people has increased in both adults and children. Researchers suggest that this rise may be linked to an increase in metabolic syndrome and obesity, both of which are associated with gallstone disease–a major trigger for pancreatic inflammation.
Symptoms of Acute Pancreatitis
Acute Pancreatitis typically presents with the following symptoms
Nausea and vomiting
Rapid Pulse
Fever
Swollen & tender abdomen
Severe abdominal pain that may
radiate to the back
Causes of Acute Pancreatitis
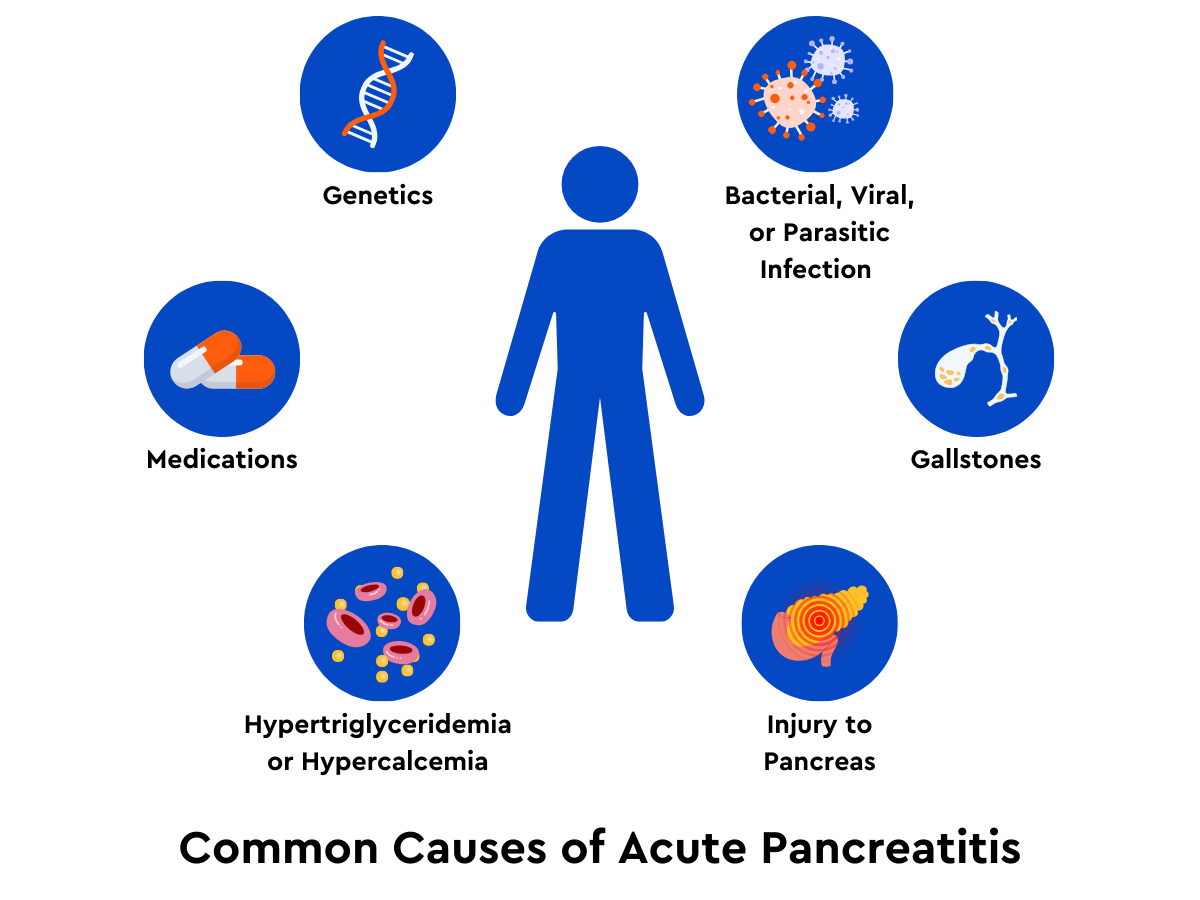
- Gallstones: The leading cause of AP. Gallstones can block the pancreatic duct, causing enzyme buildup and inflammation.
- Hypertriglyceridemia: High levels of triglycerides (a type of fat) in the blood. Read more about high triglycerides here.
- Hypercalcemia: High levels of calcium in the blood
- Medications: Certain drugs can trigger pancreatitis.
- Infections: Various viral, bacterial, and parasitic infections can trigger inflammation.
- Trauma: Physical injury to the abdomen from trauma or surgery
- Genetic factors: Some genes have been linked to an increased risk for acute pancreatitis.
- Alcohol Use? Heavy alcohol use is associated with acute pancreatitis but currently there is not enough evidence to say it directly causes AP.
Risk Factors
Alcohol Use
Long-term alcohol overconsumption (4-5+ drinks daily) can make the pancreas more sensitive to injury from other triggers such as genetics, smoking, and infections.
Smoking
Chronic and excessive smoking is a major risk factor for pancreatitis and pancreatic cancer.
Demographics
Age, gender, and ethnicity can play a role. Some studies show a higher prevalence in males and specific ethnic groups. The risk of acute pancreatitis increases with age.
Dietary habits
A high-fat diet, excessive alcohol intake, and poor nutritional habits can strain the pancreas and contribute to inflammation.
Diabetes
People with diabetes have a higher risk of developing pancreatitis. Diabetes and acute pancreatitis share many common risk factors like obesity, hypertriglyceridemia, and metabolic syndrome. A patient with one of these conditions has an increased risk for both diseases. Additionally, diabetes increases the risk of gallstones, which is a major cause of acute pancreatitis.
Ozempic and other GLP-1 RA Medications
Recent research on the link between GLP-1 Receptor Agonists (GLP-1 RAs) like Ozempic, Zepbound, Wegovy, and Mounjaro and pancreatitis is mixed. Some studies have indicated an increased risk of pancreatitis compared to other weight loss medications, while others suggest potential protective effects against AP in people with obesity or type 2 diabetes.
Individuals with a history of pancreatitis or at high risk should talk to their doctor about appropriate ways to manage diabetes and weight loss. If your doctor has prescribed Ozempic or a different GLP-1 RA, it’s important to follow their advice and recommended lifestyle changes.
Read more about Ozempic and Pancreatitis
Diagnosing Acute Pancreatitis
Diagnosis typically includes evaluating a patient’s history of symptoms and risk factors (alcohol use, gallstones, or medications) and performing medical tests. Typically, diagnosis requires 2 or more of the three criteria below.
Symptoms
Abdominal pain is a common symptom consistent with pancreatitis. Other symptoms include fluid buildup in the stomach and low blood pressure.
Blood Tests
Elevated levels of pancreatic enzymes (lipase or amylase) in the blood are an indicator of AP. In most cases, lipase levels are three times or more above the normal range.
Imaging Tests
CT scans, MRI, or ultrasound can be used to visualize inflammation of the pancreas.
Severity
As mentioned earlier, acute pancreatitis can range from mild to severe. Let’s discuss the levels of severity:
Mild Acute Pancreatitis: Usually resolves without significant complications. No organ failure or local complications.
Moderately Severe Acute Pancreatitis: May result in short-term organ failure (less than 48 hours). Moderately severe AP can sometimes include local (affecting the pancreas) or systemic (affecting the whole body) complications but generally resolves with proper treatment.
Severe Acute Pancreatitis: Characterized by prolonged organ failure (lasting more than 48 hours) and local or systemic complications. Severe AP can be life-threatening and often requires intensive care.
Complications of Acute Pancreatitis
While many cases of acute pancreatitis go away on their own, complications can occur, such as:
- Pseudocysts: Fluid-filled sacs that can form on or around the pancreas, which may require drainage if they become large or infected.
- Pancreatic necrosis: Death of pancreatic tissue.
- Infection: In severe cases, the pancreas can become infected.
- Systemic inflammatory response syndrome (SIRS): A widespread inflammatory reaction that can lead to organ failure if not treated promptly
Types of Acute Pancreatitis
AP is generally categorized into two main types based on imaging findings and the presence of pancreatic tissue death (necrosis).
Interstitial Edematous Pancreatitis:
Interstitial edematous pancreatitis is the more common and generally milder form of AP. It is characterized by pancreatic inflammation and swelling (edema) without any tissue death. The inflammation generally remains within the pancreas itself, and surrounding tissues are unaffected by it. Most cases resolve with supportive care, and most patients fully recover within a few days to weeks with no long-term complications.
Necrotizing Pancreatitis
Necrotizing pancreatitis (NP) is a more severe form of AP where pancreatic tissue dies (necrosis) due to intense inflammation and a lack of blood flow to the area. As the dead tissue breaks down, fluid collections often form in and around the pancreas. These fluid pockets can develop into pseudocysts or abscesses if they become infected:
- Pseudocysts: Fluid-filled sacs that develop in response to inflammation or tissue necrosis. They may resolve on their own, but large or persistent pseudocysts can cause symptoms or become infected, requiring drainage.
- Abscesses: Infected fluid collections that often contain pus. Abscesses are more dangerous than pseudocysts and require immediate drainage to prevent further spread of infection.
This tissue death increases the risk of complications, such as infections and multi-organ failure, making necrotizing pancreatitis a serious and potentially life-threatening condition. Patients with necrotizing pancreatitis will often need more intensive treatment and monitoring. In many cases, surgical intervention is necessary to remove the dead tissue–a procedure known as necrosectomy. However, with early diagnosis, supportive care, and timely intervention (such as drainage or necrosectomy), many patients recover.
Symptoms specific to necrotizing pancreatitis include:
- Severe, persistent abdominal pain
- Fever and chills, especially if an infection develops
- Signs of sepsis, such as low blood pressure, rapid heart rate, and difficulty breathing
- Organ failure
Treatments for Acute Pancreatitis
The main goals of treatment are to manage pain, support hydration, and nutrition needs, and address the underlying cause. Most patients require hospitalization and may receive:
- Intravenous (IV) fluids to prevent dehydration.
- Pain management with medications.
- Nutritional support, often through a feeding tube or IV nutrition if necessary.
- Treatment of underlying causes, such as removing gallstones, reducing triglyceride levels, or stopping medications that might be contributing to the inflammation.
Follow-up and Long-Term Care
Monitoring Recurrence: Preventing future episodes, which can include lifestyle changes (e.g., avoiding alcohol, managing triglycerides). An estimated 25% of patients with AP have recurrence.
Nutritional Support: Long-term dietary changes after recovery (e.g., low-fat diets, small frequent meals, and pancreatic enzyme supplements in severe cases).
Pancreatic Function Testing: Checking how the pancreas functions after recovery, including tests for diabetes.
Acute vs. Recurrent vs. Chronic Pancreatitis?
Acute vs. Recurrent Acute Pancreatitis (RAP)
A known subtype of acute pancreatitis is Recurrent Acute Pancreatitis (RAP). They are similar in their sudden inflammation of the pancreas, RAP is different because it happens repeatedly and can have more lasting effects on pancreatic health.
Acute pancreatitis: A single, isolated episode of pancreatic inflammation that often resolves fully with proper treatment and typically without lasting damage to the pancreas.
Recurrent Acute Pancreatitis (RAP): Multiple episodes of acute pancreatitis occurring over time. If you have RAP you are more likely to get chronic pancreatitis
Did you know?
An estimated 22% of people who experience one episode of acute pancreatitis may go on to develop Recurrent Acute Pancreatitis.
Acute vs. Chronic Pancreatitis
While acute pancreatitis and chronic pancreatitis both involve inflammation of the pancreas, they are different in duration and severity.
Acute Pancreatitis: Begins suddenly and usually resolves within days or weeks with proper medical treatment. It is reversible in most cases, meaning the pancreas may fully recover.
Chronic Pancreatitis: Involves repeated episodes of inflammation over time, leading to irreversible damage, scarring, and a gradual loss of pancreatic function. This condition can result in complications such as diabetes or pancreatic insufficiency.
Did you know?
An estimated 10% of people who experience one episode of acute pancreatitis may go on to develop chronic pancreatitis.
Read more about chronic pancreatitis and how to manage chronic pain.
Frequently Asked Questions
Recurrent inflammation of the pancreas, especially in chronic pancreatitis, may increase the risk of pancreatic cancer over time.
It is generally advised to avoid alcohol after an episode of AP, as alcohol is a trigger for recurrent episodes.
Episodes can last from days to weeks, depending on the severity and the patient’s response to treatment.
Frequent episodes of acute pancreatitis can increase the risk of chronic pancreatitis. Ongoing inflammation in the pancreas can eventually cause tissue scarring, impacting its ability to function properly.
Key Takeaways
- Acute pancreatitis is a sudden inflammation of the pancreas that can vary in severity.
- Common causes include gallstones, hypertriglyceridemia, infections, and damage to the pancreas.
- Symptoms include severe abdominal pain, nausea, and vomiting, and fever.
- Diagnosis involves clinical assessment and imaging studies.
Treatment focuses on supportive care and addressing underlying causes. - Complications can be severe and require careful management.
