Genetics and Pancreatitis

Recent research shows that many cases of pancreatitis have a genetic component. Historically, too much emphasis has been placed on environmental factors, such as alcohol use, in the understanding of this disease. This misconception has slowed research and the development of effective treatments, leaving many patients without answers. Today, thanks to advances in genomics (the study of genes and their function), many patients can better understand the underlying cause of their pancreatitis and the role genes play.
How Genes Cause Pancreatitis
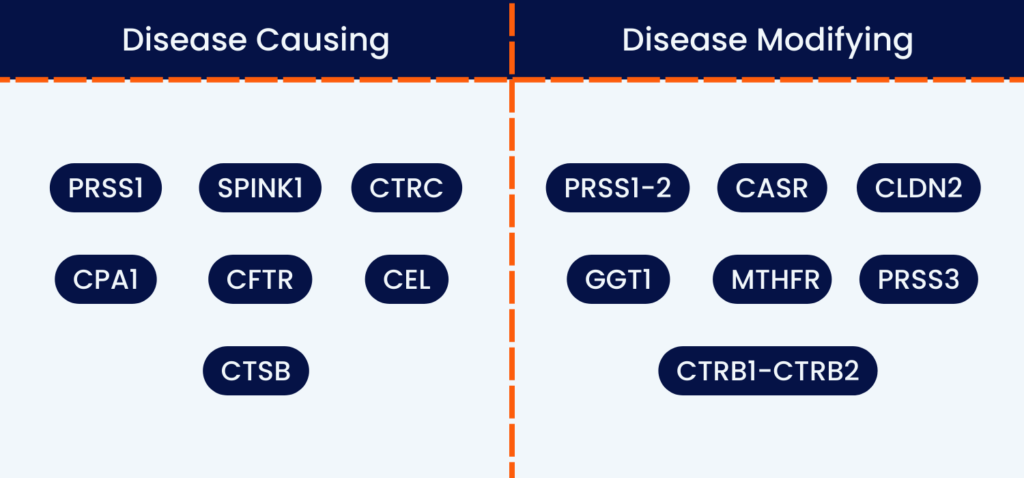
Genetic variants, meaning changes (sometimes called mutations) in the DNA, can cause or contribute to pancreatitis. The genes that play a role in pancreatitis can be classified into two groups: disease-causing and disease-modifying. Disease-causing genes are those that can directly lead to pancreatitis. On the other hand, disease-modifying genes may not cause pancreatitis on their own, but they can worsen the disease or accelerate its progression, making patients more susceptible to end-stage chronic pancreatitis characteristics. This can include cases where alcohol does play a role, as genetic factors appear to predispose patients who drink to pancreatitis.
The genes that can cause or contribute to pancreatitis include:
- PRSS1
- SPINK1
- CTRC
- CFTR
- CPA1
- CEL
- CTSB
- PRSS1-2
- CASR
- CLDN2
- GGT1
- MTHFR
- PRSS3
- CTRB1-CTRB2
How Genes Affect the Pancreas
PRSS1
The PRSS1 gene (serine protease 1) is found on the seventh chromosome and contains instructions for producing an enzyme found in the pancreas that helps break down proteins in the digestive process. When the gene is mutated, the enzyme produced is converted to its active form before leaving the pancreas and breaks down the pancreatic tissue instead of its target protein.
Have PRSS1? Join our PRSS1 Facebook Group.
Did you know?
65-80% of patients with hereditary pancreatitis have mutated PRSS1 genes.
SPINK1
SPINK1 (serine peptidase inhibitor kanzal type 1) is found on the long arm of the fifth chromosome and is commonly associated with idiopathic pancreatitis. Like the PRSS1 gene, SPINK1 codes for an enzyme produced by the pancreas that helps break down proteins in the digestive process. When the gene is mutated, the enzyme produced is converted to its active form before leaving the pancreas and breaks down the pancreatic tissue instead of its target protein.
SPINK1 mutations can be inherited genetically, but two mutated copies must be inherited in order for severe pancreatitis to develop. Most often, patients with SPINK1 mutations only have pancreatitis if they also have CFTR mutations. Because of this, SPINK1 mutations are rarely responsible for causing pancreatitis on their own.
Did you know?
2% of the general population (about 140 million people) have SPINK1 mutations.
CTRC
The CTRC gene (chymotrypsinogen C) is found on the short arm of the first chromosome and codes for a protein that protects the pancreas by breaking down prematurely activated digestive enzymes that are harmful to pancreatic tissue. When the gene is mutated, protein produced does not effectively break down the digestive enzyme, which is then free to attack the pancreatic tissue. Like SPINK1, CTRC mutations are associated with idiopathic pancreatitis.
Did you know?
CTRC mutations put you at a much higher risk of developing acute pancreatitis
CFTR
The CFTR (cystic fibrosis transmembrane conductance regulator) is found on the long arm of the seventh chromosome. It encodes a protein responsible for regulating the flow of various molecules in and out of the membranes of your lungs and other organs. When the gene is mutated, a thick layer of mucus will build up on the lining of the organs, which can lead to regular infections of lung tissue, deterioration of the pancreas, and other complications. This is known as cystic fibrosis.
Because the CFTR protein is also found in the cell membranes of cells in the pancreatic duct, a mutated CFTR gene will also affect the function of these cells. The layer of mucus produced will cause damage to the pancreatic tissue in a similar way that the lungs are affected in cystic fibrosis patients.
Did you know?
85% of cystic fibrosis patients also suffer from pancreatic insufficiency.
Watch our webinar on understanding the genetic causes of pancreatitis.
Pancreatitis in Families
What is hereditary pancreatitis?
Hereditary pancreatitis (HP) is a type of pancreatitis that is caused by variants in the PRSS1 gene. It follows a Mendelian pattern of inheritance, meaning it is passed down through a family (inherited). Hereditary pancreatitis has also been used to describe pancreatitis associated with mutations in other genes, such as SPINK1.

The Cataldos, a family affected by hereditary pancreatitis. Read Christine’s (top left) story about being diagnosed with the PRSS1 gene.
What is familial pancreatitis?
Sometimes, when 2 or more close family members have pancreatitis and the genetic cause can’t be identified, they are said to have “familial pancreatitis.” This suggests there is a genetic component.
Patients diagnosed with familial pancreatitis may actually have a known genetic cause that was not detected through their initial genetic testing. In such cases, it is important for them to explore comprehensive genetic testing options to accurately identify the genes causing or contributing to their pancreatitis.
Learn more about diagnosing pancreatitis.
Genetic Testing for Pancreatitis
Mission: Cure strongly advocates that pancreatitis patients consider genetic testing in order to identify the underlying causes of their disease and find the best treatment possible. Genetic testing will identify if you have any changes in your genes that might cause pancreatitis or result in faster disease progression, giving you and your practitioner vital information. This includes the type of disease you have, whether you have disease-modifying genes, and how your disease might progress without treatment. This information can also help determine whether any of your family members may also be at risk.
Who should get genetic testing for pancreatitis?
Any patient or clinician wanting more information about the cause of pancreatitis can seek genetic testing.
Genetic testing should be considered in pancreatitis patients who:
- Have recurrent acute pancreatitis (RAP) or chronic pancreatitis (CP) that is idiopathic (unknown cause)
- Have recurrent acute pancreatitis (RAP) or chronic pancreatitis (CP) that was diagnosed as “alcoholic pancreatitis”
- Have an early age onset of idiopathic chronic pancreatitis
- Have unexplained pancreatitis as a child (pediatric pancreatitis)
- Have a family history of idiopathic chronic pancreatitis, recurrent acute pancreatitis, or pediatric pancreatitis involving a 1st or 2nd degree family member
- Have at-risk family members of individuals with an identified pathogenic gene mutation associated with hereditary pancreatitis
Listen to Rhiannon share her experience about getting tested for hereditary pancreatitis.
What genetic tests are available?
There is a wide variety of pancreatitis testing panels offered by different companies, with some only testing for one gene and others testing for many. It is crucial to talk to your healthcare provider about your specific situation. Your doctor, and sometimes a genetic counselor, can help decide what to test and what company to use. They can explain the risks and benefits of testing and what types of results may be returned. Understanding all of this before testing is important. You can find more information about genetic counselors and find a genetic counselor here.
Available genetic testing related to pancreatitis can screen for the following:
- PRSS1
- PRSS2
- PRSS3
- SPINK1
- CTRC
- CFTR
- CEL
- CASR
- CPA1
- CLDN2
- UBR1
- SBDS
Download our genetic testing toolkit.
Understanding Genetic Testing Results
There are a number of different possible results available with genetic testing for pancreatitis. These results include:
- Positive, meaning there’s a change in one of your genes that could be associated with pancreatitis. These can be either pathogenic (known the cause pancreatitis), likely pathogenic (suspected to cause pancreatitis), or a risk allele (can increase your risk of or progression of pancreatitis).
- Negative, meaning the test did not find a genetic change known to cause pancreatitis (benign, likely benign).
- Inconclusive/Variant Uncertain Significance, meaning a mutation was found but more information is needed to understand the possible link to pancreatitis, if any.
- Unexpected, meaning a change was found in a different gene that isn’t related to pancreatitis but may be important to a different disorder.
Why Genetic Testing is Important
Traditionally, medicine has overlooked how complex acute pancreatitis and chronic pancreatitis are. This makes it difficult to find and develop therapies, and patients are often wrongly blamed for their own suffering. Medical professionals often focus too much, or solely, on the role of alcohol in pancreatitis, a role we now know has been overstated. This bias results in pancreatitis patients being offered few treatment options and little hope.
Thanks to advances in genetic testing and research, we can now understand the underlying causes of pancreatitis and how a combination of factors is involved in its development and progression. These advances are important because they increase our understanding of a long-misunderstood disease. Additionally, genetic testing can also help identify other tests that may be recommended to patients, such as screening for diabetes, cystic fibrosis, or pancreatic cancer.
In the future, genetic testing may also be able to identify which medications are most effective for patients based on their specific genetic variants. This approach is similar to what is currently done for cystic fibrosis. As more people undergo genetic testing, our understanding of the genetic and biological factors that cause pancreatitis will continue to increase. This will enable us to predict disease progression and outcomes for individual patients and provide tailored treatments to meet their specific needs. Ultimately, this will allow for earlier interventions to slow or prevent the progression of pancreatitis, moving beyond just treating symptoms.
Watch our webinar on how genes affect the medications you take.
Key Takeaways
- Pancreatitis can be directly caused by genetic variants
- The risk and progression of pancreatitis can be affected by genetic variants
- In pancreatitis patients where alcohol did play a role, genetic factors may have predisposed them to the condition
- Genetic testing is available to identify the genes related to pancreatitis and can help patients understand the necessary next steps based on results
- Genetic testing can help accelerate research and bring effective treatments to patients