Pain Management
Chronic pancreatitis (CP) is a serious condition where the pancreas is inflamed (swollen). This inflammation causes scarring of the pancreas. A big problem for people with CP is the constant pain that makes daily life hard. Knowing what kind of pain it is can help patients find the best way to deal with it.
What is chronic pain?
Chronic pain is ongoing or recurrent pain that lasts longer than the typical course of acute illness or injury or for more than 3-6 months. Chronic pain is different from acute pain. Acute pain can be considered “helpful” because it sends our body a signal that it needs to rest or change something. Usually, it goes away. The technical term for this acute pain is nociceptive pain. Chronic pain, however, is long-lasting and does not always serve a helpful function. In fact, it is harmful. Research shows that chronic pain is connected to changes in the brain. About 50 million adults are estimated to experience chronic pain in the U.S. alone!
About Chronic Pancreatitis Pain
Pain in chronic pancreatitis is a pain in the abdomen that is considered one of the most severe and debilitating types of pain. This pain is the most common symptom of chronic pancreatitis and 80-90% of patients suffer from it. Pancreatitis pain is commonly attributed to damage, inflammation (swelling) and/or irritation of the pancreas. Other factors, like social, psychosocial, and biological factors, can also play a role in chronic pancreatitis pain. In people with chronic pain, the way the body (nervous system) senses and reacts to pain might not work correctly. For example, some people feel pancreatic pain even after their pancreas has been removed during TPIAT surgery (total pancreatectomy with islet autotransplantation).
Causes of Pancreatitis Pain
Pancreatitis pain usually happens because your pancreas is inflamed, especially during flare-ups. Sometimes, it can also be caused by blockages like gallstones or cysts in your pancreas. These reasons are called “nociceptive,” which means there’s damage to tissue in the body. This pain typically feels sharp, aching, or throbbing. Often, nociceptive pain is temporary and goes away when the initial problem is fixed. For example, if your pancreatitis pain was because of a gallstone and the pain stopped after removing the gallstone, it would be called nociceptive pain.
Additionally, when the pancreas becomes physically inflamed and damaged (scarred), it can cause the nerves of the pancreas to become damaged too. This causes a type of pain called neuropathic pain, also known as nerve pain. When the nerve fibers become damaged, they can send pain signals to the brain, even when you may not be experiencing a pancreatitis flare or when your pancreas is in a relatively “normal” state.
Other Factors Contributing to Pancreatitis Pain
The cause of pain in chronic pancreatitis patients is complex and can be different from person to person. Not only can the physical characteristics (inflammation and damage) of chronic pancreatitis cause pain, but biological factors, social factors, and physiological factors can all play a role. This is explained by the biopsychosocial understanding of pain. Health habits such as sleep, smoking, physical activity, health beliefs, and substance use can also affect pain.
Where is Pancreatitis Pain Felt?
Pancreatitis pain is located in the upper abdomen, usually on the left side. It can also spread to the stomach, back, chest, ribs, and lower left shoulder blade. It is generally described as a burning, aching pain that gradually gets worse over time. It may also flare up several minutes after eating or drinking.
Listen to Dr. Steven D. Freedman, MD, Ph.D., explain:
- The causes of pancreatic pain
- How pancreatic pain is evaluated
- Non-invasive treatment options for chronic pancreatitis pain
Managing Chronic Pancreatitis Pain
Pancreatitis can cause extreme pain and make daily activities difficult. Although there isn’t a cure yet, there are many ways to help manage the pain. It’s important to have a healthcare provider comprehensively assess your pain to determine the most effective treatment. It is best if the doctor specializes in gastrointestinal pain, but unfortunately, there aren’t enough of these specialists. Treatment can include a combination of pain education, pharmacological therapy (medicine), and psychological interventions (therapy). Complementary and alternative therapies, such as yoga and massage therapy, may also help.
Guidelines for Managing Pancreatitis Pain
Current guidelines recommend clinicians approach pain management through a series of steps. These steps include:
- For patients determined to have pain primarily from their pancreas:
- Stop smoking and alcohol, optimize nutrition
- Consider endoscopy if there are stones or strictures
- Start treatment with acetaminophen or NSAID in selected cases
- Consider non-coated enzymes or combine with antioxidants
- Follow the patients!
- If pain is not relieved, conduct psychological evaluation and, if warranted, treat with appropriate medications (SSRI, TCA, SNRI) and/or cognitive behavioral therapy.
- If pain is not relieved, conduct neurophysiological evaluation where possible.
- If “segmental hyperalgesia” is found, treat with gabapentinoids
- If “deficient descending inhibition” is found, treat with tricyclic antidepressives (TCA)
- Or serotonin-noradrenalin reuptake inhibitors (SNRI)
- If pain is not relieved, treat with weak opioids such as tramadol and codeine & follow patient
- If pain is not relieved, consider strong opioids & follow the patient in order to taper down again later:
- Use slow-release preparation
Rotate opioids - Watch for opioid-induced bowel dysfunction & taper or treat with laxatives
- Consider new combination therapies, alternative treatments such as ketamine, transcranial magnetic stimulation, and acupuncture.
- Use slow-release preparation
If you don’t have access to a healthcare provider who specializes in pancreatitis pain, we encourage you to share these guidelines with your doctor so they can better manage your pain.
Learn more about the recommended approach to treating pancreatitis pain.
Medication
Pain medication can be used to treat pancreatitis pain with the guidance of a doctor. Pain medications include steroids, anti-inflammatory painkillers, mild painkillers, stronger painkillers, opioids, and nerve blockers. Typically, doctors will recommend milder painkillers before moving on to stronger painkillers and other medications to treat pancreatitis pain.
Learn more about medications for pancreatitis pain.
Pancreatic Enzyme Replacement Therapy (PERT)
PERT comes in two forms: uncoated and coated. Uncoated PERT may help reduce chronic pancreatitis pain in some patients. An example of uncoated PERT that has shown to be effective for pancreatitis pain includes Viokace. PERTs work to mimic the function of the pancreas by improving fat and protein absorption in exocrine pancreatic insufficiency (EPI). Please know that other PERTs, while effective for EPI, have not shown to be effective for pancreatitis pain.
Procedures and Surgeries
Certain procedures and surgeries may be considered to help alleviate pancreatitis pain. Whether you are a suitable candidate for a surgical procedure needs to be thoroughly assessed by you and a pancreas specialist.
Surgeries and procedures used to relieve pancreatitis pain include:
- Endoscopic retrograde cholangiopancreatography (ERCP). Endoscopic therapy may be considered as a treatment option for pancreatitis caused by strictures or stones if other medical therapies fail and pain persists. Endoscopic therapy (ERCP), uses a scope that goes down to the pancreatic duct to remove stones or place stents across strictures; however, an ERCP can cause pancreatitis and this risk must be carefully considered.
- Extracorporeal Shock Wave Lithotripsy (ESWL). Extracorporeal shock wave lithotripsy is a procedure to break up stones inside the bile ducts or pancreatic duct with a series of shock waves generated by a machine called a lithotripter. The goal of the procedure is to break the stones into smaller pieces that can pass through the body or become easier to extract.
- Gallbladder removal surgery (Cholecystectomy). Gallbladder removal surgery may be a treatment option if pancreatitis pain is caused by gallstones.
- Whipple procedure (Pancreaticoduodenectomy). Whipple procedure is a surgery that removes inflammation and masses located on the head of the pancreas. It is most commonly used to treat pancreatic cancer but is also used to remove cysts in the bile duct and scarring in the pancreas. However, it may also remove a large amount of the surrounding tissue, increasing the risk of diabetes or causing other complications.
- Puestow Procedure (Longitudinal Pancreaticojejunostomy). The Puestow procedure is used to treat chronic pancreatitis by draining the duct of an inflamed pancreas. It does not require the removal of the pancreas or the duodenum.
- Frey Procedure. The Frey procedure is a new type of surgery that involves a combination of draining the pancreatic duct along with the removal of pancreatic tissue. It is recommended for patients who have pancreatitis caused by blockage in the head of the pancreas.
- Total Pancreatectomy with Islet Auto Transplantation (TPIAT). The TPIAT is an extreme surgery that involves the full removal of the pancreas and transplanting the patient’s own pancreatic islet cells into the liver. It is primarily for people with recurrent acute and chronic pancreatitis.
Medical Cannabis
Medical cannabis, also referred to as medical marijuana, may be helpful to improve the quality of life for pancreatitis patients experiencing severe pain. Medical marijuana can be used for chronic pancreatitis patients experiencing pain, anxiety associated with the pain, and nausea, and to stimulate appetite. Research has suggested that it may decrease the amount of opioid use and lessen the number of hospitalizations.
Medical marijuana is legal in 38 states and the District of Columbia, but it is not legal federally. It comes in a variety of forms, including edibles, vaping, smoking, oils, and powders.
Listen to Dr. Tim Gardner, MD, MS, FACG explain:
- How medical cannabis can be used to treat pain
- The correct dosing, strain (CBD vs. THC), and recommended intake form for medical marijuana
- Legal issues regarding obtaining medical cannabis
- The potential risks associated with medical marijuana
Lifestyle Changes
Changing daily habits may help you manage pancreatitis pain. These habits can include physical activity, getting enough sleep, and relaxation strategies.
Diet
Changes to your diet can help reduce pain. Many experts recommend that pancreatitis patients eat a low-fat, high-protein diet that stays between 30 to 50 grams of fat per day (in the U.S.), although the guidance is different in Europe. Other recommendations include not drinking alcohol, avoiding butters and oils, and spreading out your food and snacks into smaller meals throughout the day. These changes can help your pancreas better digest food and minimize the risk of a flare.
Learn more about nutrition for chronic pancreatitis.
Physical Exercise
Physical exercise has been shown to improve overall health. It can also decrease pain, nausea, anxiety, and stress. There are many ways to exercise, like walking, jogging, stretching, and swimming. Try to exercise for 45 minutes, three times a week. Change your daily exercise to add some movement, but make sure to pay attention to how much energy you have and how much pain you feel. Remember, talk to your doctor before starting any hard exercise.
Self-Care
Taking care of yourself when dealing with pancreatitis pain goes beyond just medical treatments. It’s about looking at the bigger picture and finding ways to make yourself feel better. Self-care includes strategies and habits that can help you manage the discomfort and challenges that come with pancreatitis. By learning and practicing these strategies, you can feel better overall and have more control over your pain.
Self-care practices for pancreatitis pain include:
- Yoga. Yoga is a combination of physical and mental exercise that combines deep breathing exercises and concentration practices with gentle physical exercise. Research has shown that yoga can improve the quality of life in pancreatitis patients.
- Massage Therapy. Massage therapy manipulates the body’s tissues by using physical touch. It is used to treat pain and stress.
- Meditation. Meditation is the practice of mindfulness by training one’s mental attention and awareness. It involves positioning your body in the most comfortable position and then becoming aware of your thoughts. Meditation can last anywhere from 10 minutes to several hours.
- Acupuncture. Acupuncture is a form of alternative medicine that stimulates special acupuncture points in the body to release the body’s natural pain-killing chemicals into the muscle system and brain. There are many ways to stimulate acupuncture points. The most common is through thin, metallic needles inserted into the skin or through electrical stimulation.
- Journaling. Journaling can help those experiencing pain by providing an outlet for thoughts and emotions. It can be used as a tool by those experiencing chronic pain to help record symptoms, emotions, and experiences.
The Burden of Pancreatitis Pain
Chronic pain can impact the lives of people who suffer from it in many different ways and place additional burdens on patients and their caregivers.
Burden on Daily Life Activities
Patients with pancreatitis pain can have reduced physical functioning, which means that certain activities can become difficult or impossible. Some patients have problems sleeping and fulfilling their roles in social settings or at work. In general, it can be challenging to function socially. Pain can also reduce the psychological functioning and well-being of patients. For example, chronic pain can cause stress, worries, and anxiety. Unfortunately, depression is common among people who suffer from chronic pain. Chronic pancreatitis patients may also experience frequent doctor appointments or hospitalizations.
Financial Burden
Chronic pancreatitis is associated with a severe cost burden. As chronic pancreatitis is a long-term disease, treatment, medication, and hospitalization costs can add up over time. A study in 2016 found that the average medical cost for chronic pancreatitis patients was $40,589 per year. This figure included hospitalization, outpatient and pain medications, surgery, and endoscopic retrograde cholangiopancreatography. The study also found that chronic pancreatitis patients annually spend about $614 on pain medications, $1,761 on diabetic medications, and $4,114 on pancreatic enzyme replacement therapy.
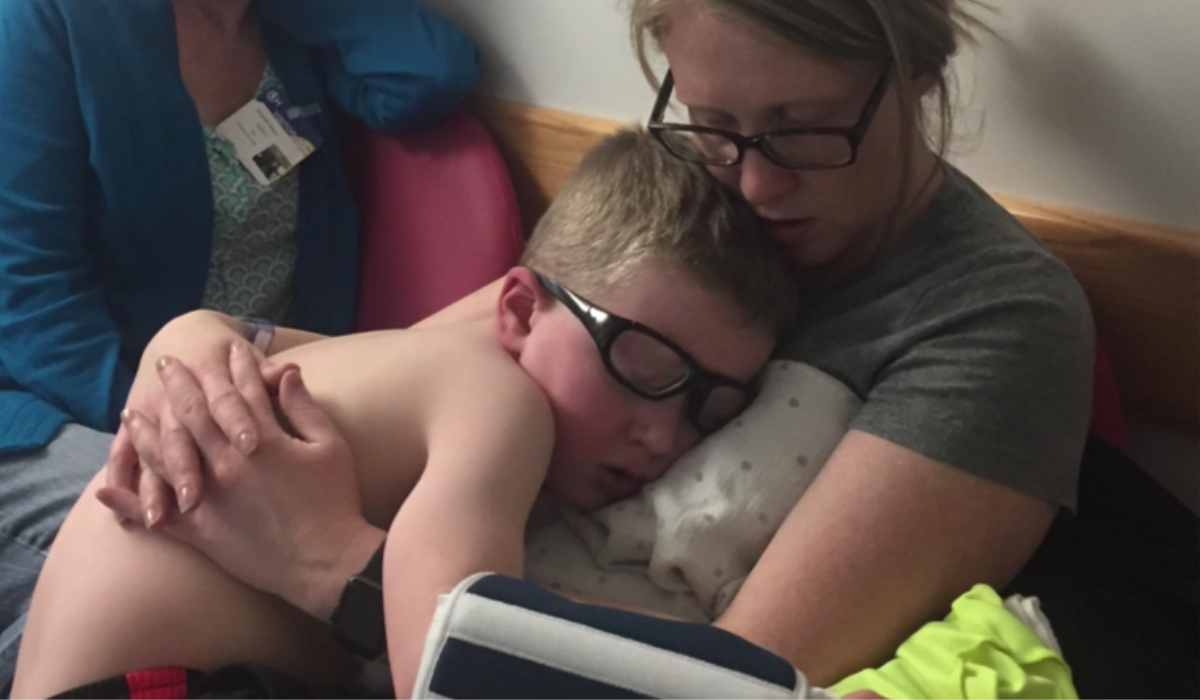
Burden on Children and Caregivers
If a child suffers from pain, it can affect parents and the whole family. Children suffering from pain might struggle to attend school and perform well. Parents and caregivers also have their own emotional responses to the diagnosis and management of their child or loved one’s chronic pain. Many feel discouraged by the lack of a clear diagnosis or a treatment plan and are angry, worried, and/or fearful about their child or loved one’s condition.
Learn more about pediatric pancreatitis.
Assessing Pancreatitis Pain
Chronic pain is complicated and difficult to assess and treat. A broad assessment is necessary in order to create a comprehensive treatment. The following factors of the pain should be considered:
- Intensity/severity
- Location
- Duration, frequency
- Quality – neuropathic (pain that comes from damage to the nervous system) vs nociceptive (pain that comes from injury or disease)
The pain system is complex and involves the brain. Looking at the brain can give important insights into how pain is caused and modulated. For example, we know that adult pancreatitis patients are more sensitive to pressure pain and have impaired pain modulation (pain signals to the brain).
Pain Scales for Chronic Pancreatitis
A pain scale is a tool used by physicians and medical providers to assess a patient’s pain. However, not all pain scales can capture the full pain experience. It is important to know how pain impacts the individual person in order to assess the pain. Since anxiety and depression are very common among chronic pain patients, relevant symptoms should be addressed.
There are many different types of pain scales. The following is a list of the most commonly used pain scales for chronic pancreatitis:
- 0-10 Numeric Pain Rating Scale. The 0-10 numeric pain rating scale is a generic measure of pain intensity and is used for a variety of different medical situations. 0 indicates no pain, while 10 indicates the worst amount of pain possible.
- Short-form 12 (SF-12). The SF-12 pain scale is a general measure of pain intensity and health-related quality of life. It consists of 12 questions and is scaled from 0-100, with 0 indicating no pain, and 100 indicating the worst pain possible. It is recommended for use for pancreatitis by the International Study Group for Pancreatic Surgery. While its questionnaire is not specific to pancreatitis, it has been shown to consistently and accurately measure changes in pain levels and treatment response.
- Short-form Comprehensive Pain Assessment Tool (COMPAT). COMPAT is a pain scale designed specifically to assess pain for those experiencing chronic pancreatitis. It consists of 6 questions that measure various aspects of chronic pancreatitis pain, as well as the quality of life, pain patterns and severity, and other factors influencing pain. Pain is scaled from 0-100, with 0 indicating no pain, and 100 indicating the worst pain possible.
It is important to recognize that each person experiences pain differently. Pain scales, especially with respect to pancreatitis, cannot capture the full impact of pain.
Pain Management Resources
Johns Hopkins Pancreatitis Pain Program
The Johns Hopkins Pancreatitis Pain Program is a research initiative and patient care outreach center that aims to better understand and personalize pancreatitis pain treatment. Its team consists of physicians, mental health specialists, psychiatrists, and neurogastroenterologists to provide holistic treatment to improve chronic pain. Learn more about the Johns Hopkins Pancreatitis Pain Program.
Clinical Trials
There are several clinical trials studying treatments for pancreatitis. These studies aim to develop effective treatments. Learn more about what is involved in these pancreatitis clinical trials to see if they are right for you.
Latest Pain Management Blog Posts
Easing Chronic Pancreatitis Pain | Johns Hopkins Pancreatitis Pain Program
In this Mission: Cure patient education webinar, Dr. Speed and Dr. Treisman discuss the Johns Hopkins Pancreatitis Pain Program. Pain is a difficult and often

New Collaboration with Johns Hopkins to Treat Pancreatitis Pain
Mission: Cure has provided initial funding to Johns Hopkins Medicine to launch the new Pancreatitis Pain Research Center. Mission: Cure will work with Johns Hopkins
Key Takeaways
- Chronic pancreatitis pain is constant or recurrent pain that can make daily life hard. It generally occurs as a burning, aching sensation in the upper abdomen, but may also spread to other parts of the body, like the back and chest.
- Pancreatitis pain can be caused by many factors including inflammation of the pancreas, obstruction of the pancreatic duct, or nerve damage. Biological, social, and psychosocial factors also contribute to pain.
- There are several different types of treatment available for managing chronic pancreatitis pain. These include medications, medical therapies and surgeries, medical cannabis, and lifestyle changes.
- Pancreatitis can put a burden on patients’ overall mental and physical health, their finances, and their family and caregivers. However, there are resources available for managing pancreatitis pain.
- Pancreatitis pain can be measured using pain scales. However, each person experiences pain differently and pain scales may not measure the full experience of pain.
