Ozempic, a medication used to manage type 2 diabetes, falls under a category of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists. While it effectively lowers blood sugar levels, there are concerns about its potential to cause pancreatic inflammation, or pancreatitis. This blog post, guided by Dr. Melena Bellin, an expert in diabetes and pancreatitis, explores the relationship between GLP-1 receptor agonists like Ozempic and pancreatitis
What is Pancreatitis?
Pancreatitis is the swelling (inflammation) of the pancreas, an organ responsible for making hormones such as insulin and glucagon to control blood sugar levels. The condition varies from mild, temporary cases to more serious cases that require hospitalization and intensive medical attention. There are three types of pancreatitis:
- Acute Pancreatitis (AP). Acute pancreatitis is a single episode of inflammation of the pancreas. It’s often sudden and extremely painful but only occurs over a short period (from days to a week).
- Recurrent Acute Pancreatitis (RAP). Recurrent acute pancreatitis is the result of repeated episodes of acute inflammation of the pancreas, with complete recovery in between episodes. Patients with RAP have a higher risk of developing chronic pancreatitis.
- Chronic Pancreatitis (CP). Chronic pancreatitis is a long-term, progressive condition characterized by the persistent inflammation of the pancreas. This leads to permanent damage and scarring that weakens the pancreas. Consequently, you may experience digestive problems and other complications, such as diabetes and bone disease.
Many types of medications, including Ozempic, have been linked to pancreatitis. However, it is difficult to diagnose drug-induced pancreatitis, and researchers are still working to understand exactly how these drugs trigger inflammation in the pancreas.
What is Ozempic?
Ozempic, also known by its generic name semaglutide, is a prescription medication used to treat type 2 diabetes and obesity. Administered as a once-weekly injection, it helps lower blood sugar levels and supports weight loss.
How does Ozempic work?
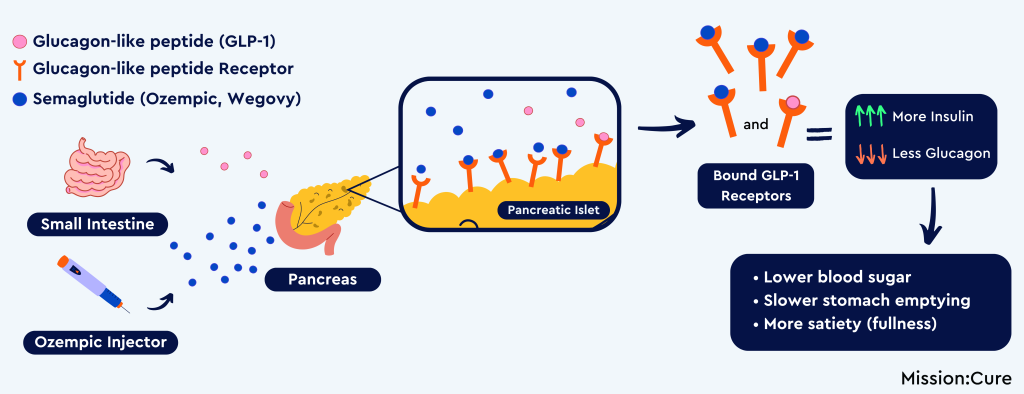
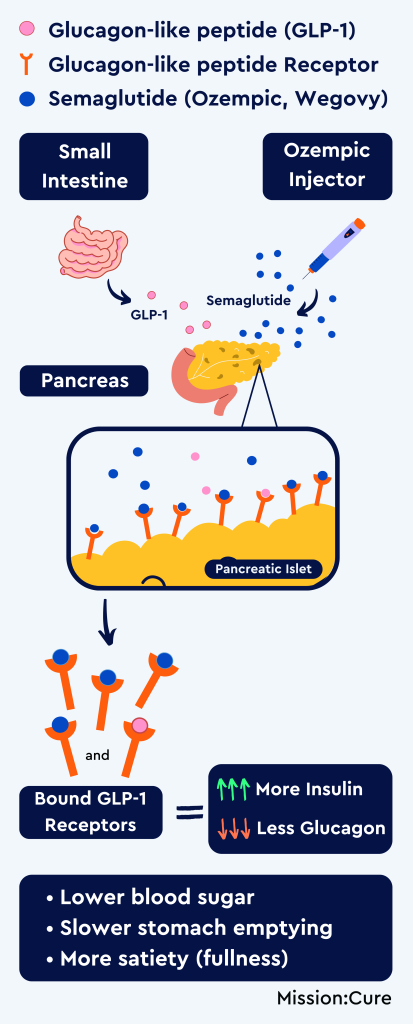
Glucagon-like peptide (GLP-1) is a hormone made in the small intestine, and it plays many roles in the body. One of these roles is to stimulate the pancreas to release insulin, an important hormone for regulating blood sugar levels. Additionally, the GLP-1 hormone lowers the amount of glucagon released by the pancreas. Glucagon is a hormone that would otherwise raise blood sugar levels by prompting the release of glucose (sugar) from the liver. This dual mechanism helps prevent spikes in blood sugar levels and slows gastric (stomach) emptying. By maintaining stable blood sugar levels, GLP-1 also helps to regulate appetite and the feeling of fullness (satiety) after eating.


Ozempic is a medication in the class of drugs known as glucagon-like peptide-1 (GLP-1) agonists. These agonists mimic the action of the hormone glucagon-like peptide (GLP-1) by selectively binding to and activating the GLP-1 receptor. As a result, they stimulate insulin secretion, inhibit glucagon release, slow gastric emptying, and promote a feeling of satiety, thereby helping to regulate blood sugar levels and support weight loss. GLP-1 agonists are not a cure for type 2 diabetes or obesity. People should use them alongside dietary and lifestyle changes. While Ozempic (semaglutide, Wegovy) may be the most well recognized by name, other similar drugs acting on the GLP-1 pathway exist as daily or weekly injections, or as a pill (Rybelsus).
Pharmaceutical companies have recently introduced newer medications that mimic the action of both GLP-1 and another gut hormone called GIP. These new agents marketed as Mounjaro or Zepbound (generic Tirzepatide) can also treat type 2 diabetes, and they may have an even greater impact on weight loss.
Ozempic for Type 2 Diabetes
In type 2 diabetes, the body cannot effectively regulate blood sugar levels, often due to insulin resistance or inefficient insulin production. When blood sugar levels start to rise after eating, GLP-1 agonists stimulate the body to make more insulin. By increasing insulin release, Ozempic helps regulate the rate your body absorbs glucose and nutrients into the bloodstream, lowering blood sugar levels.
Another significant advantage of GLP-1 agonists is their cardiovascular benefits. Studies have shown that these medications can reduce the risk of major adverse cardiovascular events, such as heart attacks and strokes, in individuals with type 2 diabetes. This makes them a valuable component of a comprehensive diabetes management plan.
Ozempic for Weight Loss
Clinical trials, where researchers compare a medication to a placebo (or ‘fake medication’), have demonstrated the effectiveness of GLP-1 agonists in promoting weight loss. Patients treated with these medications have achieved average weight losses ranging from 5% to 15% of their initial body weight over several months. These are significant reductions in body weight compared to those that received a placebo. However, the degree of weight loss varies based on the specific medication used, dosage, and individual patient characteristics.
Semaglutide received FDA approval for weight loss under the brand name Wegovy in cases where diet and exercise are ineffective. Wegovy comes as a weekly injection used for chronic weight management. Despite the different name, it is essentially the same medication used to treat diabetes. Like Ozempic, Wegovy slows digestion and increases feelings of fullness by mimicking the GLP-1 hormone. As a result, the person will be less hungry and somewhat lower their food intake. By making it easier to stick to a low-calorie diet, Wegovy supports long-term lifestyle changes needed for sustained weight loss.
Wegovy vs. Ozempic
Unlike Ozempic, Wegovy’s formula contains higher doses tailored for weight loss purposes. Conversely, Ozempic, designed for type 2 diabetes management, contains lower doses of semaglutide. Although Ozempic is commonly covered by health insurance plans, they may not always include Wegovy in insurance coverage. This difference can impact treatment decisions and accessibility for patients seeking weight management solutions.


Side Effects of Ozempic
While GLP-1 medications are effective in managing diabetes and obesity, they can cause side effects, with gastrointestinal (GI) issues being the most common. Nausea and vomiting are frequently reported among these GI side effects.
Other side effects of Ozempic include:
- Constipation
- Stomach (abdominal) pain
- Changes in vision
- Low blood sugar (hypoglycemia)
- Kidney problems (kidney failure)
- Possible thyroid tumors, including cancer
- Possible gastroparesis may also rarely be associated with gallstones or acute pancreatitis
- Pancreatic inflammation
Given the potential for serious side effects, it’s crucial to be aware of the risks associated with Ozempic, particularly the risk of pancreatitis.
Read more about potential side effects
Does Ozempic Cause Pancreatitis?
Though it is uncommon, there have been instances of people developing pancreatitis due to the use of Ozempic. For those with a history of pancreatitis, Ozempic and similar medications might be potential triggers.
To study a medication’s side effects, researchers run randomized clinical trials, where they compare the drug to a placebo (a fake medicine) in a controlled way. Clinical trials on Semaglutide haven’t shown more cases of pancreatitis than in people who took a placebo or no treatment. Combining data from many trials with Ozempic or similar drugs shows no evidence that the risk of developing acute pancreatitis increases. However, there are some important limits to consider with clinical trials:
- Eligibility Criteria. Clinical trials have specific eligibility criteria and often exclude high-risk patients. For example, those with a history of pancreatitis were not included in these studies, limiting the generalizability of these findings.
- Duration of Follow-up. Clinical trials typically follow patients for short periods (months to a year or two), which may not be enough to capture long-term treatment risks.
- Rare Occurrence of Acute Pancreatitis. Acute pancreatitis is relatively rare, requiring a large number (many thousands) of study participants to see an effect.
How Common Is Pancreatitis With Ozempic?
Since multiple factors can contribute to pancreatitis development, researchers are unsure if cases with Ozempic are due to chance. Factors such as prior medical history or genetic predispositions can influence the likelihood of pancreatitis while using Ozempic. Medications like Ozempic can also raise the risk of gallstones, as rapid weight loss and potential effects on the gallbladder contribute to this risk. Gallstones can, in turn, increase the risk of acute pancreatitis.
Some epidemiological studies on how often diseases occur suggest that people using older versions of daily injected GLP-1 medications for type 2 diabetes may have double the risk of getting acute pancreatitis. This risk can be higher when using these drugs for weight loss. A recent large study showed a nine-times higher risk compared to other weight loss drugs. However, in general, acute pancreatitis affects about 1 in 2,500 adults each year. So, while there is some risk with medications like Ozempic, it remains low for most people.
On the other hand, weight loss and treating type 2 diabetes might help protect against acute pancreatitis. A recent study using data from a large population found that in patients who had a past episode of acute pancreatitis, those treated with this class of medications had fewer recurrences compared to those taking other type 2 diabetes medications.
Symptoms of Pancreatitis While On Ozempic
Symptoms of pancreatitis can vary in severity and may manifest differently for each person. While taking Ozempic, it is important to keep an eye out for any signs of pancreatitis and seek immediate medical attention if you experience any of the following symptoms:


- Severe pain in the upper abdomen that may radiate to the back
- Fever
- Rapid heart rate
- Nausea and vomiting
- Inability to eat or drink
- Jaundice (yellowing of the skin or whites of the eyes)
If you have any of these symptoms, especially severe stomach pain while taking Ozempic, you should get medical help or go to the emergency room right away. Doctors can diagnose acute pancreatitis by checking for high levels of pancreatic enzymes (like lipase or amylase) in your blood. They may also use imaging tests, like a CT scan or MRI, to look for inflammation caused by acute pancreatitis.
Who’s Most At Risk For Pancreatitis While Taking Ozempic?
Researchers need to conduct more studies to identify which groups are at the highest risk of developing pancreatitis while using Ozempic. However, those with conditions like diabetes, obesity, and gallstones are believed to have a higher likelihood of getting pancreatitis.

The Risk Of Pancreatitis With Type 2 Diabetes
Although diabetes doesn’t directly cause pancreatitis, people with type 2 diabetes are at a higher risk of developing it. This is due to the pancreas either not producing enough insulin or the body not using insulin properly. Since Ozempic treats diabetes, it’s unclear whether GLP-1 analogs, the diabetes itself, or both contribute to the risk of pancreatitis. Researchers need to conduct more studies to understand how these medications and diabetes are linked to pancreatitis.
Can You Take Ozempic If You Have Pancreatitis?
If you have a history of recurring acute or chronic pancreatitis, using Ozempic or similar medications may make pancreatic inflammation worse and is generally not recommended. Individuals at risk for pancreatitis should talk to their doctor about other ways to manage diabetes and weight loss, like lifestyle changes, diet, or different medications.
If your doctor has prescribed Ozempic, it’s important to follow their advice and recommended lifestyle changes. Work closely with your doctor to slowly adjust the dose, as increasing it too quickly can raise the risk of side effects, including pancreatitis.
What Next: Pancreatitis Diagnosis When Taking Ozempic?
If you’re taking Ozempic (or similar medications) and have an episode of acute pancreatitis, your doctor will likely advise you to stop the medication. Based on your test results and symptoms, they may suggest switching to a different treatment permanently. However, if the diagnosis is unclear, your doctor might recommend restarting Ozempic with close monitoring.
It’s usually safe to stop Ozempic suddenly without tapering, but always talk to your doctor before making any changes. The chances of having another pancreatitis episode after the first one aren’t well understood. If you have severe pain or vomiting, get medical help right away. While nausea is common with Ozempic, discuss any worrisome symptoms with your doctor.
Key Takeaways
- Pancreatitis, which is inflammation of the pancreas, is a rare but serious side effect of Ozempic.
- Ozempic may increase the risk of pancreatitis, especially for people with risk factors like diabetes, obesity, and gallstones. Identifying those at higher risk helps doctors monitor patients better.
- If you develop pancreatitis while using Ozempic, your doctor will likely recommend stopping the medication. However, this decision should be made together, based on your specific situation.
- Researchers need to conduct more studies to understand the link between Ozempic and pancreatitis and to find effective ways to prevent and manage it in at-risk individuals.
About Mission: Cure
At Mission: Cure, we are dedicated to finding effective treatments and, ultimately, a cure for pancreatitis. Through patient education, research, and advocacy, we strive to improve the lives of those affected by this condition.
Don't Miss Out!
Read Our Blog: Dive deeper into the topics that matter to you. Our blog features expert insights, recent studies, and stories from the pancreatitis community.
Engage in Our Community Forum: Health Unlocked is a space for open discussion on everything pancreatitis-related. Whether you’re seeking advice or offering it, we welcome you.
Share Your Story: Sharing your experience can inspire and encourage others facing similar challenges.
Join Facebook Support Groups: Connect with others who understand what you’re going through in our Facebook support groups.