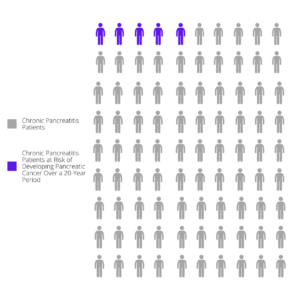
Having chronic pancreatitis increases the risk of pancreatic cancer. According to Dr. Randall Brand, Gastroenterologist and head of the early pancreatic cancer detection program at the University of Pittsburgh Medical Center, people with chronic pancreatitis have approximately a five percent chance of developing pancreatic cancer over a 20-year period. [1]
However, recent research has shown that the risk is not evenly distributed among chronic pancreatitis patients. People with PRSS1 variants (sometimes called hereditary pancreatitis) have a significantly increased risk of pancreatic cancer, although it is hard to accurately quantify the risk because different research studies have shown different risk levels. Studies suggest that people with chronic pancreatitis and some CFTR mutations and chronic pancreatitis have a slightly greater risk of pancreatic cancer than the general population. Thus far, research has not found a direct association or increased risk for pancreatic cancer for people with chronic pancreatitis-linked genetic variants such as SPINK1, CTRC and CEL but there needs to be more research on other genetic variants, chronic pancreatitis and pancreatic cancer. [2]
How can pancreatic cancer be detected early when it can be removed through surgery?
The challenge is that—so far—there is no screening test to detect early stage pancreatic cancer. Screening for pancreatic cancer involves imaging the pancreas through procedures like Magnetic Resonance Imaging (MRI) and endoscopic ultrasound (EUS). And, because tumors within the pancreas are difficult to see, even with these types of scans, these tests are not 100% accurate. Because pancreatic screening tests are invasive, expensive and only partially accurate, experts agree that only people with a high risk of pancreatic cancer should be routinely screened.
Two new sets of guidelines on pancreatic cancer screening were published in 2020: The American Gastroenterology Association Clinical Practice Update on Pancreas Cancer Screening in High-Risk Individuals; Expert Review and International Consensus Guidelines on Surveillance for Pancreatic Cancer in Chronic Pancreatitis.
Key Recommendations for Pancreatic Cancer Screening
Here are the key recommendations summarized from both of the new guidelines:
1. People with PRSS1 “hereditary” pancreatitis should be screened for pancreatic cancer.
Specific mutations in the PRSS1 gene have been identified as a cause of recurrent acute or chronic pancreatitis. People with this mutation usually have pancreatitis symptoms by age 20.
When should people with PRSS1 pancreatitis be screened for pancreatic cancer?
Experts recommend that in the absence of other symptoms or risk factors, patients get screened starting at age 40. Screening should be repeated every 12 months assuming no concerning pancreatic lesions are found.
What does pancreatic cancer screening involve?
The American Gastroenterological Association (AGA) recommends that screening should be done by a combination of MRI and endoscopic ultrasound (EUS). However, the guidelines from the international pancreas associations (IAP, APA, JPS, EPC) noted that it can be difficult to detect early pancreatic cancer through EUS in patients with chronic pancreatitis because pancreatic inflammation, fibrosis, and calcifications caused by pancreatitis can make it difficult to accurately identify and classify cancer tissue. This guideline recommends computed tomography (CT) scans. The American Cancer Society best describes these tests.
2. People with pancreatitis and SPINK1 p. N34S variants do not have a high enough risk of pancreatic cancer to warrant screening.
3. Patients with chronic pancreatitis associated with other mutations, including CFTR, CTRC, CPA1 and CEL, do not have a high enough risk of pancreatic cancer to justify screening or surveillance.
NOTE: Many people with chronic pancreatitis get MRI’s, EUS, or CT scans when their pancreatitis symptoms warrant these tests for diagnostic or therapeutic purposes. In those cases, doctors should look for signs of pancreatic cancer or pre-cancerous lesions. The pancreatic cancer screening in this article is for people who would not otherwise get these screening tests.
4. Patients with pancreatic cancer-related genetic variants should be screened
The AGA guidelines recommend screening for people with other known pancreatic cancer-related genetic variants, such as BRCA1, BRCA2. For these groups, screening should start at age 50.
5. People with two or more blood relatives with pancreatic cancer should be screened
The AGA recommends screening for people who have two or more blood relatives, including one immediate family member, with pancreatic cancer even if they don’t have an identified genetic mutation. For these people, screening should start at age 50 or 10 years before the age at which a family member was diagnosed.
For patients with chronic pancreatitis, genetic testing can identify any pancreatic cancer-linked genetic mutations. Genetic tests can also help you and your doctor better understand if genetics are causing or contributing to your chronic pancreatitis.
Both sets of guidelines agree that pancreatic cancer screening is not useful and should not be performed if pancreatic resection (surgery) is not a viable option for that particular person.
Aside from getting screened, what can you do to prevent pancreatic cancer? [3]
- Avoid smoking
- Maintain a healthy diet high in fruits and vegetables
- Follow a regular exercise routine
- Lose weight if necessary
There are ongoing efforts to develop better, less invasive screening tools such as blood tests, to identify pancreatic cancer early. Until such tools become available, those of us with an increased risk for pancreatic cancer should be screened once each year.
Want to learn more about symptoms and treatment of pancreatic cancer? Please review the information provided by Pancreatic Cancer Action Network.
Key Takeaways
- Pancreatic cancer is very rare. But it is also very deadly because by the time it is discovered, it often has already started to spread to other organs.
- People with pancreatitis and a PRSS1 genetic mutation (hereditary pancreatitis) should be screened every year for pancreatic cancer starting at age 40.
- Screening involves an MRI and a CT Scan.
- Annual pancreatic cancer screening is not currently recommended for pancreatitis patients with SPINK1 p. N34S, CFTR, CTRC, CPA1 and CEL genetic mutations unless they have two blood relatives with pancreatic cancer.
- Stopping smoking, a healthy diet, and exercise can help prevent pancreatic cancer.
- If you do not know what genetic mutations you have, you can find out through specialized genetic testing.
[1] Ariel Precision Medicine and National Pancreas Foundation Webinar: Why Does Someone Develop Pancreatic Cancer? Oct. 28, 2020, https://www.youtube.com/watch?v=n_wR-UwJn4U&t=425s
[2] Cazacu, Irina Mihaela, et al. “Pancreatitis-Associated Genes and Pancreatic Cancer Risk.” Pancreas, vol. 47, no. 9, 2018, pp. 1078–1086., doi:10.1097/mpa.0000000000001145. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6291258/pdf/mpa-47-1078.pdf
[3] Brand RE, Lerch MM, Rubinstein WS, et al. Advances in counselling and surveillance of patients at risk for pancreatic cancer. Gut. 2007;56(10):1460-1469. doi:10.1136/gut.2006.108456 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2000231/

