Have you ever wondered if your pancreatitis flares may be connected to your monthly periods? You’re not alone in making this connection. While menstrual cycles are part of the reproductive system, they can impact other parts of our body – including the pancreas. In this blog post, we’ll explore this possible connection with insights from Dr. Steven Freedman, a pancreatic disease and cystic fibrosis expert at Harvard Medical School.
What is Pancreatitis?
Pancreatitis is typically split into three types: acute pancreatitis, recurrent acute pancreatitis, and chronic pancreatitis.
- Acute Pancreatitis. Acute pancreatitis (AP) is a single episode of inflammation of the pancreas. It’s often sudden and extremely painful. Most people who have an episode of acute pancreatitis will start to feel better within a week and have no further problems.
- Recurrent Acute Pancreatitis. Recurrent acute pancreatitis (RAP) is repeated episodes of acute inflammation of the pancreas. In RAP, patients have two or more acute pancreatitis episodes and completely recover between episodes. Patients with RAP have a higher risk of developing chronic pancreatitis.
- Chronic Pancreatitis. Chronic pancreatitis (CP) is an ongoing inflammation of the pancreas, leading to scarring that damages the organ. As a result, the pancreas no longer works properly, causing problems with digestion and leading to exocrine pancreatic insufficiency, diabetes, and bone disease.
Some people with recurrent acute pancreatitis and chronic pancreatitis may notice symptoms and flares around their monthly cycle. However, acute pancreatitis is unlikely to have any impact on your menstrual cycle.
What is a Period?
A period (also referred to as menstruation) is a part of the menstrual cycle where bleeding occurs from the vagina. During a period, the body discards blood and tissue from the uterus (womb) through the vagina. Generally, periods occur every month, for about 5 days.
Women, girls, and trans-masculine people can menstruate. Typically, Periods begin at the age of 12 and stop occurring around the age of 52.
What Happens During the Menstrual Cycle?
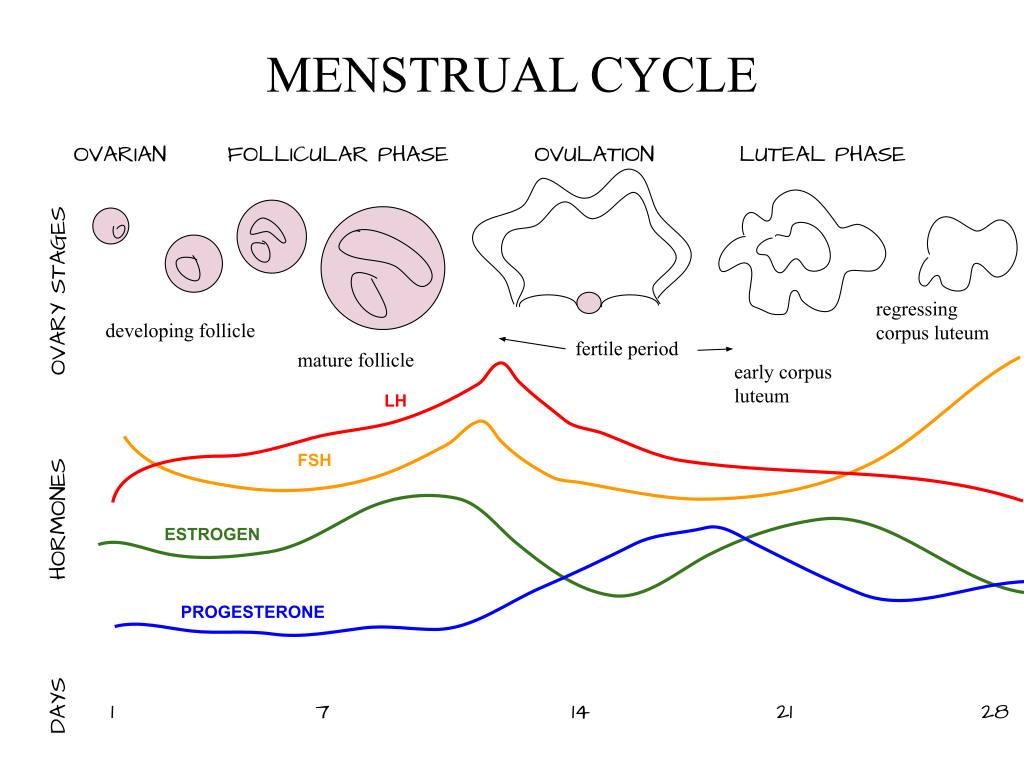
The menstrual cycle is a monthly hormonal process that happens as the body prepares for possible pregnancy. A typical cycle lasts approximately 28 days, from the first day of one period to the first day of the next, although this can vary from one person to another. During this time, the pituitary gland and the ovaries create and release hormones at different stages of the cycle.
The Cycle Consists of 4 Stages
- The Menses Phase. The uterine lining begins to shed in response to a decline in estrogen and progesterone. This occurs on the first day of the menstrual cycle.
- The Follicular Phase. This is the longest phase of the menstrual cycle. As an egg develops in the ovaries, estrogen levels increase, causing the uterine lining to grow and thicken.
- Ovulation. Ovulation occurs with the help of the luteinizing hormone (LH). As LH levels increase, the ovary releases an egg
- The Luteal Phase. Progesterone levels, as well as estrogen levels, increase to prepare the uterine lining for pregnancy. If pregnancy does not occur, estrogen and progesterone levels drop and the uterine lining sheds during a period.
Common Symptoms During Menstruation
Some symptoms during your period can mimic symptoms during a pancreatitis flare. If you’re ever unsure whether your period or pancreatitis is causing a symptom, talk to your doctor.
Common symptoms during menstruation include:
- Abdominal or pelvic cramping
- Bloating
- Food cravings
- Mood swings
- Muscle aches
- Fatigue
- Headache
- Trouble sleeping
Pancreatitis and Periods: Can Pancreatitis Affect the Menstrual Cycle?
Is there a connection between pancreatitis and periods? Though research is limited, it suggests that people who menstruate and are prone to pancreatitis may flare-up during estrogen peaks throughout the menstrual cycle.
First, let’s discuss the relevance of the cystic fibrosis transmembrane conductance regulator (CFTR) gene. While the CFTR gene is most commonly associated with cystic fibrosis, a condition that causes thick mucus to build up in multiple organs, it can also cause chronic pancreatitis.

The CFTR gene controls the CFTR protein, which manages the flow of salt and water in cells that produce mucus, sweat, and digestive enzymes. When estrogen levels peak during the menstrual cycle, they disrupt CFTR protein functions. This disruption leads to more mucus building up in the body for at least one week of the cycle.
As a result, if you have CFTR-related pancreatitis, when estrogen levels peak during your menstrual cycle, it may cause more mucus to build up in and around your pancreas. This mucus can block the digestive enzymes produced by the pancreas, making them get “stuck” instead of releasing into the duodenum (the first part of the small intestine). This blockage can cause inflammation in your pancreas.
Hormonal changes during menstruation can also influence the severity of pancreatitis symptoms. As mentioned before, estrogen and progesterone levels change during the menstrual cycle. Estrogen tends to increase the speed of digestion, whereas progesterone does the opposite. When these hormones go out of balance, it can affect the secretion of digestive enzymes from the pancreas and may lead to either gallstones, inflammation, or both.
Learn more about new research involving the CFTR gene.
Genetic Testing
If you are unsure if you have the CFTR gene, strongly consider talking to your doctor about genetic testing. Genetic testing will identify any changes in your genes that might cause pancreatitis or result in faster disease progression.
This gives you and your doctor important information, including:
- The type of disease you have
- Whether you have disease-modifying genes
- How your disease might progress without treatment.
- Whether your family members may also be at risk
Learn more about genetics and pancreatitis.
More Things to Consider
Estrogen therapy, like birth control pills or hormone replacement therapy (HRT), is a rare cause of acute pancreatitis. Though it is not certain if estrogen therapy directly causes pancreatitis, the potential risks should be considered for those with preexisting conditions or other known risk factors for chronic pancreatitis.
Hormone Replacement Therapy (HRT) and Pancreatitis

Hormone replacement therapy (HRT) is a type of medication that contains estrogen. Doctors commonly use it to treat menopause symptoms by boosting low estrogen levels. However, there are certain risks associated with this type of treatment depending on your own health factors.
In one report, a transgender patient using HRT was taken to an emergency room due to severe abdominal pain, nausea, and vomiting. Upon examination, she was diagnosed with acute pancreatitis. After treatment and stopping estrogen therapy, her symptoms completely cleared up. Other cases similar to this one have been reported, and more research is necessary to understand the role HRT may play in causing acute pancreatitis.
Birth Control and Pancreatitis
Birth control pills contain hormones that help regulate the menstrual cycle and ease PMS symptoms. Though estrogen-containing birth control is generally considered safe, it can increase cholesterol levels in the liver. This extra cholesterol can build up in bile and lead to the production of gallstones, which is a risk factor for pancreatitis.
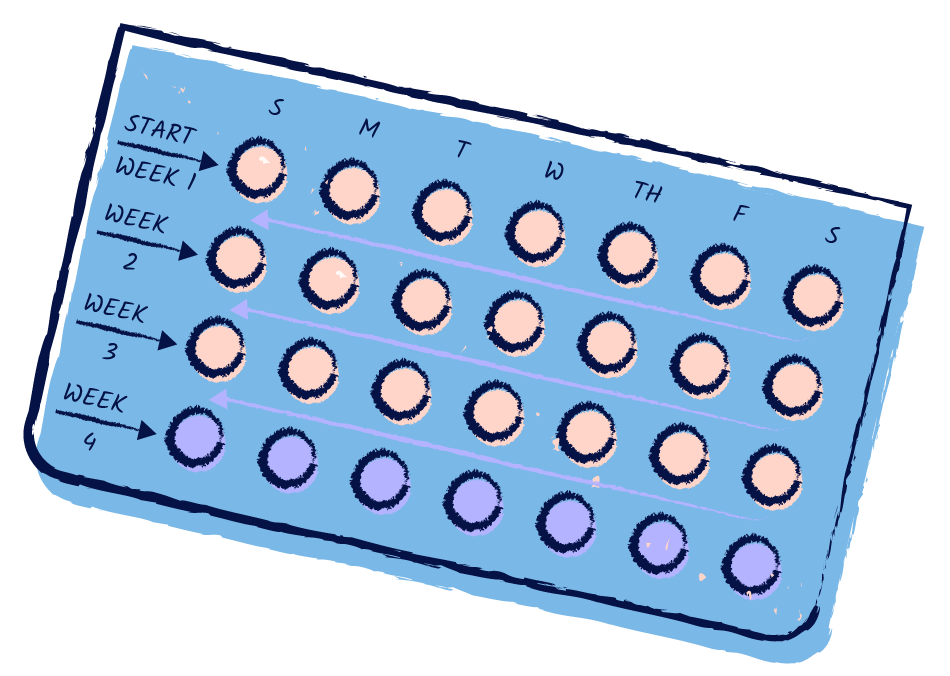
In another case, estrogen was found to increase the levels of fatty substances in the blood. When these substances are sent to the pancreas to be broken down, they can cause damage, inflammation, and ultimately, pancreatitis. This is especially true in people with a higher risk of pancreatitis or other risk factors.
What Patients Have To Say
We asked our patient community on HealthUnlocked whether they thought their periods impacted their pancreatitis. Here’s what they had to say:
“My flares of pancreatitis were definitely linked to my menstrual cycle and hormone changes. I had been experiencing heavy periods and severe pain after the birth of my first child, which they tried to solve [by] stopping my menstrual cycle with contraceptive injections. When on the injections, my digestive issues also reduced; each time I came off [them, my symptoms] got worse as my cycle began again.”
“Unlike when I had a menstrual cycle, I get flares three to four times a year which I can quite easily bring back under control, rather than having 12/13 bouts a year which were outside my control before my hysterectomy.”
“I had terrible problems with periods and have been on hormone pills and more recently injections for most of my life, so I am not certain because I used to get so many problems all at once! I did notice I would get what I now know is steatorrhea each month and crippling pain so it’s probable [it’s linked to pancreatitis] but I can’t be definitive.”
Therapy Options
While there is no direct link between estrogen and pancreatitis, research suggests that estrogen can trigger inflammation and damage the pancreas. Using anti-estrogen medications may be a therapeutic treatment your doctor can consider to manage symptoms associated with pancreatitis. However, the effectiveness of this treatment can vary based on individual factors and the underlying cause.
If you are considering anti-estrogen medication treatment, talk to your doctor. They can help you weigh the potential benefits and risks based on your medical history and needs.
How can I tell the difference between period symptoms and pancreatitis symptoms?
High levels of estrogen can cause symptoms like irregular or heavy periods, weight gain, and fatigue, which may impact the severity of pancreatitis attacks. In people predisposed to pancreatitis, hormonal fluctuations may trigger or worsen pancreatic inflammation.
Pancreatitis shares some similar symptoms with menstruation, but the main thing to watch out for is severe pain in the upper belly that may radiate to the back. You might also experience a fever, belly tenderness, and a rapid pulse. Pancreatitis may also worsen digestive issues, leading to symptoms such as nausea, vomiting, and diarrhea.
Advice for Getting Through Pancreatitis and Periods
Managing both periods and pancreatitis can be challenging. It is important to maintain a healthy lifestyle, including a balanced diet and regular exercise. Additionally, practicing self-care, such as managing stress and getting enough rest, can minimize the impact of both menstruation and pancreatitis on overall well-being. It is important to work closely with a healthcare provider to develop a personalized plan for managing both conditions.
Key Takeaways
- Hormonal changes during the menstrual cycle can indirectly cause more severe pancreatitis symptoms for some people, particularly those with CFTR genetic mutations.
- When estrogen levels peak, it can lead to increased mucus production. This may cause digestive enzymes to build up in the pancreas, resulting in inflammation.
- Genetic variations, especially in the CFTR gene, can predispose a person to pancreatitis. Genetic testing can provide insights into pancreatitis risk and/or progression.
- Estrogen-containing medications, while generally considered safe, can cause flare-ups and the development of acute pancreatitis. Research suggests anti-estrogen medications could relieve inflammation and pancreatic symptoms.
Stay Up-To-Date on the Latest Pancreatitis Advancements
Mission: Cure is a coalition of patients, doctors, researchers, and entrepreneurs. We are pioneering a new approach to curing diseases through innovative, outcome-based financing. Headquartered in New York City and operating virtually, Mission: Cure collaborates with researchers, innovators, and impact investors to discover life-altering therapies and bring them to patients. Currently, Mission: Cure is focused on accelerating a cure for pancreatitis. Support Mission: Cure by donating, and stay up-to-date with the latest pancreatitis news by subscribing to Mission: Cure’s newsletter, following Mission: Cure on Facebook, Instagram, Twitter, and LinkedIn, and subscribing to its YouTube Channel. Join Mission: Cure’s pancreatitis communities on HealthUnlocked and Facebook.

