Preventing Diabetes:
Q: Is there anything a chronic pancreatitis patient can do to prevent or reduce the risk of diabetes?
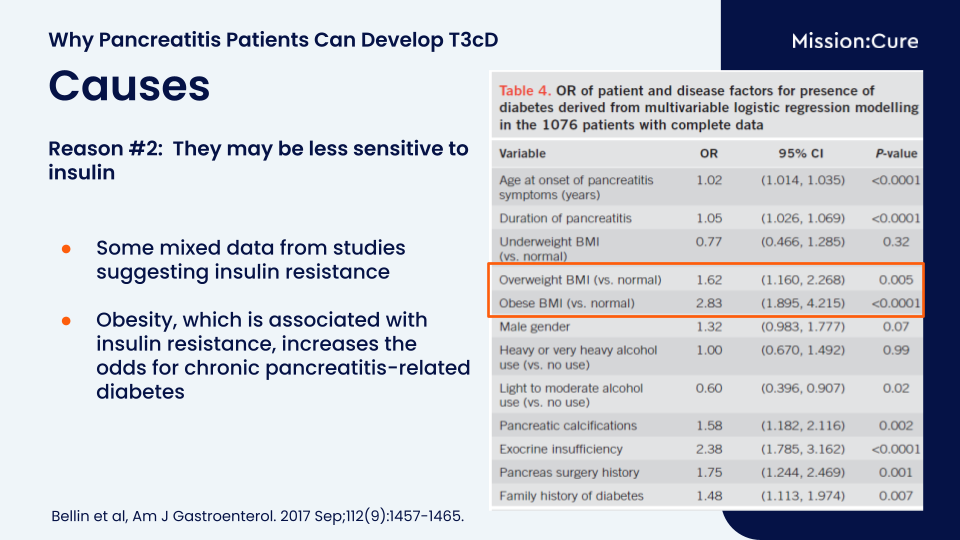
A: Not everyone with CP will get diabetes in their lifespan. In terms of prevention, we know that obesity increases your risk of getting diabetes even with pancreatitis. So, maintaining a healthy body weight and staying physically active, if you’re able, may help lower the risk of diabetes. There is not a therapy yet to prevent progression to diabetes.
Possible Treatment Options:
Q: Does creon help decrease pancreatitis attacks - like does it help reduce stress on pancreas? Or no correlation.
A: The evidence is lacking. Most studies in adults suggest Creon does not help decrease attacks, but Viokase, which doesn’t have an enteric coating might (but the data are again mixed). They may help though for pain symptoms if someone also has maldigestion from exocrine insufficiency.
Q: EPI - is Creon the only treatment?
A: Pancreatic enzymes made from pig enzymes are the only treatment for exocrine insufficiency right now. There are several different brands on the market. The only other option is a cartridge called Relizorb that hooks onto tube feeds for people who are getting tube feeds (can’t be used for food that you eat).
Read more about Pancreatic Enzyme Replacement Therapy (PERT)
Q: Does taking Pancreatic Enzymes help or hurt short term and long term?
Q: What is your opinion on using Berberine?
Q: What treatment do you recommend: insulin pump vs injections? Is one insulin better than another? How to deal with morning highs?
A: It depends on the person. For some people who do well on basal insulin injections, the easiest thing is to do insulin injections.Some people— those who require multiple daily injections, are insulin-sensitive, or are young children needing small doses—tend to do well with an insulin pump. There is no one answer of which is better.
For the morning high, there are many different reasons why this could be happening. One reason is due to the cortisol changes. Our cortisol is in a circadian type of rhythm that rises overnight and peaks in the morning. The rise of cortisol (which raises blood sugars) can affect the overnight and morning blood sugar. For some people, the morning high could be the cortisol effect. There could be other reasons. In order to deal with this, a pump may be a good option because you can set the insulin delivery throughout the day. In terms of different types/brands of insulin.
For most people, the brand of the long-acting insulin and rapid-acting insulin does not matter much. Some of the long-acting insulin brands will last longer than others, so some people would react better to one of the long-acting insulin brands than the other. Every once in a while, someone is better responsive to a certain rapid acting insulin than another, so mostly the brands are interchangeable.
Specific Cases
Q: I had the TPIAT in 2010 at UofMN Fairview- I had about 320,00 yield but my islets seem to have a mind of their own. My BG shoots up to 250+ then crashes to under 65 within 50 min. My dexcom looks like a roller coaster ride. Any suggestions?
A: It is complicated, because it may seem like your islets are functioning well in the sense you can come off insulin therapy, and yet you have these kinds of highs and lows. Some of the reasoning for the “roller coaster ride” can be due to the gut surgery part of TPIAT – which changes the GLP-1 and incretin hormones. Also, if islets are slow, it might take longer to kick in after having a meal, so there are highs and lows.
Q: PRSS1 - acute and chronic 12 yo male - how often do you recommend MRCPs? Also, should C-Peptides be drawn to the yearly lab work?
Q: Is there a connection between acute necrotizing pancreatitis & osteoporosis? I’ve had a diagnosis of osteopenia for 6 years.
A: Yes, or at least in chronic pancreatitis it is well established that risk for osteopenia and osteoporosis are increased. It is probably a risk with necrotizing pancreatitis for the same reasons. Nutritional deficiency, malabsorption (especially low vitamin D levels), inflammation and in some cases inactivity due to illness may all contribute.
Read more about how pancreatitis affects nutritional deficiencies and bone disease
Q: I am in the Boston area. I have CP dx a year ago. My A1c is normal or near normal. But I have frequent symptoms of hypoglycemia. I tested it on my home monitor. Also have many many hypoglycemic sx. I cannot find a doctor to address this. My CP doc dismisses it. How can I find a knowledgeable doctor for this in the Boston area?
A: We do sometimes see hypoglycemia in patients with CP. It could be due to undernutrition, prolonged fasting, or associated with pancreatic surgeries, or caused by reasons we don’t yet understand. True hypoglycemia is <70 mg/dL with symptoms or <54 mg/dL in someone without diabetes, but a few people will be more sensitive and may have low symptoms at a higher threshold. For evaluation you could ask for referral to an endocrinologist who sees patients with hypoglycemia, or a diabetes specialist.
Q: Is it better to live with a CP with multiple acute attacks and T3C or to have the pancreas removed and be T1?
A: The answer for this may be different for different people, so it is a good question to discuss with your doctors. If you consider a total pancreatectomy, you can have a consult evaluation (which does not require you to have surgery) to get more information.
Q: Probably a very strange one. Our son had a very high thirst throughout his pancreatitis journey - minimum requirement of 5 liters per day and on one occasion in hospital consumed 10 liters in a 24 hour period. Alongside this he gained 70 lbs in a 2 year period, he also has Hashimotos. His HbA1c was checked throughout but was fine. Strangely when he had his TPIAT his thirst returned to normal as has his weight - is this normal?
A: It is not typical (but that’s not to say it is abnormal). I’m not sure why your son had these symptoms. Thirst and urine output are tightly regulated in our body to keep the right balance of water and sodium in our blood. Some people engage in behavioral drinking, meaning they simply tend to drink a lot. This can sometimes lead to a cycle where they continue drinking excessively because the kidneys stop concentrating urine as effectively. As a result, they feel the need to keep drinking to stay hydrated.
Q: Re: GLP-1 agonists, can you explain the mechanism that might create or effect pancreatitis?
This is a bit difficult to answer because the studies vary in whether or not these agents truly cause pancreatitis, and how high that risk is. However, we do see some stimulation of the exocrine pancreas with the GLP-1 agonists, and there are GLP-1 receptors on the exocrine cells. This is presumably why patients with type 2 diabetes in clinical trials have about a 2-fold increase in lipase levels on treatment, and may be a mechanism for acute pancreatitis risk. Rapid weight loss can also increase the risk of gallstones forming, which can then cause gallstone pancreatitis.
Q: I am now supplementing with IV infusions to help with nutritional deficits. I’m already prescribed Creon in a rather large dose and although it helps with digestion, my tests show I’m still not absorbing enough nutrients.
Given the relationship between exocrine dysfunction and T3c, I’m wondering if there’s any benefit to supplementing with IV to help manage the endocrine dysfunction? I’ve read that science isn’t sure whether the call on insulin - via incretin - (associated with the attrition process of digestion) is a cause or an effect of T3c…. I would imagine this could make a difference as to whether or not IV infusions may or may not help.
A: I don’t have any data on IV infusions of vitamins. TPN (or nutrition through the vein) which is sometimes used, has some vitamins in it. For most people, what we recommend for vitamins are special vitamins made for those without a pancreas. These are formulations like MVW, AquaDEKs, and DEKAs. In fact, the company that makes Creon has a program called Creononcourse.com where some individuals on Creon may be able to get vitamins for free. These vitamins are formulated so that vitamins A, D, E, and K can be absorbed without normal fat digestion. They also contain much higher doses than standard multivitamins, which often makes them more effective than typical options you’d find on the shelf.
Learn more about Vitamins and Pancreatitis
Q: Hi from a sunny but nippy Ireland. Just wondering, our son had his TPIAT 4 months ago and a 630,000 islet yield was achieved which we are delighted about. Currently he is only on background insulin and is reducing this. Is there an average lifespan of islets in the liver? Is there anything we should be prepared for? Thanks so much
A: We know that most people who come off insulin stay off for 2-5 years then gradually go back on. There are a number of individuals who do stay off insulin >10 years, and I am aware of only a couple of cases out to ~20 years.
Q: My daughter had a feeding tube placed due to having chronic pancreatitis and she passed away 9 months after this. Could the feeding tube have exacerbated her symptoms?
A: I am so sorry for your loss. Feeding tubes are common in chronic pancreatitis, and for many (but not all) people they help with the symptoms (reduce pain or nausea).
Q: I had endometriosis at a very early age and had to have a hysterectomy at the age of 23. Could any of that have an effect on having pancreatitis and diabetes later in life?
A: This will probably not affect pancreatitis or diabetes directly. However, if ovaries were removed (oophrectomy) at the time of hysterectomy, do consider screening for bone health with a bone density scan. Individuals with pancreatitis and diabetes have a higher risk for low bone mineral density. Estrogen is one of the most important hormones for building bone strength, so surgical removal of the ovaries or early menopause might increase this risk.
Learn more about bone disease and pancreatitis
Q: PRSS1 acute and chronic pancreatitis - any specific diet recommendations?
A: Balancing diet in pancreatitis can be complicated as people’s daily calorie needs, absorption, activity level, and “safe” foods (those that reduce pancreatitis symptoms) vary. If considering how to reduce risk of diabetes long-term, the best diet is one that helps maintain a body mass index in the normal range (around 20-25 kg/m2).
Learn more about nutrition and pancreatitis
Pancreatitis and COVID
Q: Have you seen any correlation to Pancreatitis and COVID? I have no formal diagnosis yet but have been found to have EPI and am now prediabetic (A1C of 5.7). I was very healthy prior to contracting COVID over a year ago. Since I’ve had daily abdominal discomfort and poor digestion. My doctors said there seems to be pancreatic damage and have me scheduled for an MRI.
More Information
Q: Dr. Bellin had LIFT listed as one of the organizations at the end of her talk. Can you share what this organization is?
A: Good eye! This is a study Dr. Bellin is leading. Click here to find out more information on the LIFT trial!
Q: Do you know of any endocrinologists in the US or UK comfortable with Type 3c Diabetes?
A: Because providers and centers can change over time, I’d suggest starting with a center that has a large comprehensive pancreatitis program or a total pancreatectomy islet autotransplant program, if available in your area, as a resource for endocrinology care in pancreatitis-related diabetes.
Technical Webinar Questions:
Q: Will you be addressing type 3c due to surgery and not only pancreatitis?
A: Most of the material should apply to people who have Type 3c due to surgery. Dr. Bellin sees patients like that all the time!
The 3 following questions refer to the “Causes – Reason #2″ slide from the webinar. Watch it here: 21:00-22:20
Q: Are risk factors cumulative or is that not the correct interpretation? For instance, if you are male (1.32) and have Exocrine Insufficiency (2.38), would your total risk be 3.7 times higher?
A: It’s a good question, but no, you can’t add up these numbers. Each factor was considered separately.
Q: Should the for Age of onset of Pancreatitis symptoms (years) be interpreted? Is the 1.02 types age at diagnosis?
A: That means for every year of age older you were at the time that pancreatitis was diagnosed, your risk for diabetes increases by 2% (which may just be because older people are more likely to have diabetes in general)
Q: Duration of Pancreatitis, is the total risk 1.05 x number of years?
A: For every extra year that you have pancreatitis your risk goes up by 5%
Stay Up-To-Date on the Latest Pancreatitis Advancements
Mission: Cure is a coalition of patients, doctors, researchers, and entrepreneurs. We are pioneering a new approach to curing diseases through innovative, outcome-based financing. Headquartered in New York City and operating virtually, Mission: Cure collaborates with researchers, innovators, and impact investors to discover life-altering therapies and bring them to patients. Currently, Mission: Cure is focused on accelerating a cure for pancreatitis. Support Mission: Cure by donating, and stay up-to-date with the latest pancreatitis news by subscribing to Mission: Cure’s newsletter, following Mission: Cure on Facebook, Instagram, Twitter, and LinkedIn, and subscribing to its YouTube Channel. Join Mission: Cure’s pancreatitis communities on HealthUnlocked and Facebook.